
Understanding how to put effective health care into practice is an important part of the effort to improve the population’s health. Implementation science aims to address this, and draws on a range of research methods to help us understand how health organisations can effect change and, importantly, the barriers to making changes.
Members of PenCLAHRC's Implementation Science team have been working with the South West Academic Health Science Network (SWAHSN) to study how two projects – the emergency treatment of acute ischaemic stroke and patient-initiated clinics (PIC) – have sought to spread innovation. In both projects, work was initially conducted in one setting and shown to be effective, and so considered ready to be rolled out across the region. In practice, however, implementation following these projects was problematic and wasn’t as successful as had been anticipated.
The ASPIC study was launched to try to understand the differences in context of spread in the Acute Stroke and the PIC projects within local hospitals, and to identify cross-cutting lessons for future work. Using a qualitative approach, and drawing on a relevant framework from implementation science, the study ultimately aimed to recognise the critical factors helping and hindering the implementation of the ‘best practice’ identified by projects.
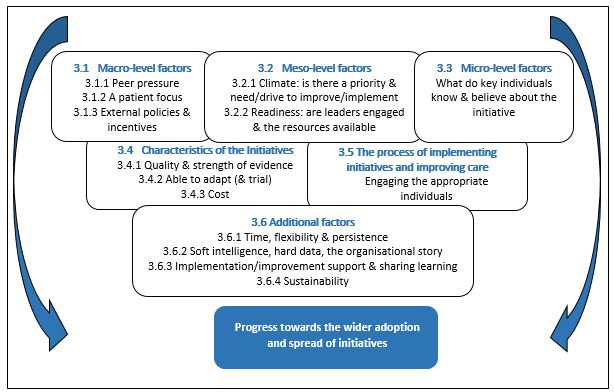
Findings demonstrated that the most important influences on implementation occurred at the organisational, department and team level. Critical factors included the priority, need or drive for change, and readiness in terms of skilled leadership (particularly from the clinical leads) and available resources.
 Cross-cutting critical factors influencing spread
Cross-cutting critical factors influencing spread
Other critical influential factors included a competitive pressure to improve, a patient focus, engaging key individuals, creating space to reflect on progress, external facilitation and support. It was found that a lack of influential external national and regional policy and incentives to support the work had an impact on success. The availability of strong evidence for change was important but not always a dominant factor in the process of spread.
The team found that project members and key individuals in each setting had to be persistent, flexible in their approach, and given time to do this work. There is a benefit to collecting ‘hard data’ on performance and outcomes, and ‘soft intelligence’ on the psycho-social-emotional factors helping and hindering the spread of implementation and improvements.
Project lead, Dr Jo Day, commented that:
"This study provided a valuable opportunity to generate insights as to how context influences the wider spread of evidence-based practice in acute settings. We identified critical cross-cutting factors, informed by work from Implementation Science, across both projects. This provided 18 lessons which can be used to assist similar future collaborative projects to enhance care and the patient experience in the South West."
The team developed these lessons into a checklist, using questions such as ‘Are there any external drivers that support or undermine the change or improvement?’ and ‘Is the team sufficiently stable to make changes and do you know their workload pressures?’ These questions highlight the fact that further work is needed to identify existing strategies and resources to develop, nurture and sustain organisational, team or department readiness for change. Considering this, the next steps for the team include working with the SWAHSN to develop ‘phase two’ of the project, which will be focused on building upon these findings, developing resources, and potentially testing approaches to support implementation.
The ASPIC research summary report is now available.
You can read more about the ASPIC study on our project page.
